Many of the more critical proteins in the process are membrane-bound, in particular the Min proteins, which in E. coli accumulate at the cells poles and prevent formation of the FtsZ ring anywhere but the centre of the cell:

A very simple diagram showing the Min proteins in fuzzy blue at the poles, and the FtsZ ring in red in the centre of the cell. This ring then contracts to create two bacterial cells.
So a group of researchers in Newcastle were working on the Min system and looking at it by immobilising the bacteria on slides which were covered in a layer of polylysine. They were finding it very difficult to actually get this localisation of the min proteins, rather than being membrane bound at the poles the protein was all over the place. They did a few more tries and eventually realised that it was the polylysine that was causing the problem. Adding polylysine to cells trying to divide slowed the process right down as it stopped the Min from properly localising.What polylysine does to cells is affect the proton-motive force (pmf), which is used by bacteria to produce energy.
 Diagram shows a stylised version of proton motive force at the bottom of the bacteria. Ions are pumped through the membrane creating energy in the form of ATP. Image taken from Osaka university website.
Diagram shows a stylised version of proton motive force at the bottom of the bacteria. Ions are pumped through the membrane creating energy in the form of ATP. Image taken from Osaka university website.In order to verify that the crazy-behaving Min proteins were due to the polylysine affecting the pmf they tried using slides covered with other pmf-blockers such as CCCP, which is actually a bacterial poison as it kills the pmf completely (and before people start enquiring about its use as an antibiotic, bear in mind it's also a human poison, for the same reason). The results were clear, when CCCP is absent the Min clusters at the poles of the dividing bacteria, when it's present the Min is diffused throughout the cells:

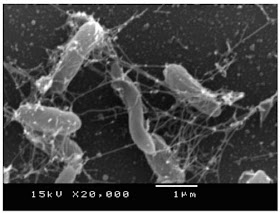
Cells in the absence (on the left) and the presence (on the right) of CCCP. MinD is attached to GFP, which is bright. Image from the reference.

Cells in the absence (on the left) and the presence (on the right) of CCCP. MinD is attached to GFP, which is bright. Image from the reference.
In the figure above (from the reference) you can see the Min in the poles of the dividing cells on the left and in no particular orientation on the right. Killing the pmf leads to lack of arrangement of the proteins required for cell division. This affect was shown to be independent of the concentration of ATP in the cell, so it's not just that the lack of energy is preventing protein attachment, it's that the Min proteins rely on the correct ion concentration across the membrane in order to attach.
The moral of the story: Sometimes things don't work for exciting reasons!
(The other moral of the story: always wash your slides :p)
The moral of the story: Sometimes things don't work for exciting reasons!
(The other moral of the story: always wash your slides :p)